Davenport, F. M. & Hennessy, A. V. Predetermination by infection and by vaccination of antibody response to influenza virus vaccines. J. Exp. Med. 106, 835–850 (1957).
Google Scholar
Davenport, F. M., Hennessy, A. V., Stuart-Harris, C. H. & Francis, T. Jr. Epidemiology of influenza; comparative serological observations in England and the United States. Lancet 269, 469–474 (1955).
Google Scholar
Jensen, K. E., Davenport, F. M., Hennessy, A. V. & Francis, T. Jr. Characterization of influenza antibodies by serum absorption. J. Exp. Med. 104, 199–209 (1956).
Google Scholar
de St Groth, F. & Webster, R. G. Disquisitions of original antigenic sin. I. Evidence in man. J. Exp. Med. 124, 331–345 (1966).
Google Scholar
Hoskins, T. W., Davies, J., Smith, A. J., Miller, C. & Allchin, A. Assessment of inactivated influenza-A vaccine after three outbreaks of influenza A at Christ’s Hospital. Lancet 313, 33–35 (1979).
Google Scholar
Keitel, W. A., Cate, T. R. & Couch, R. B. Efficacy of sequential annual vaccination with inactivated influenza virus vaccine. Am. J. Epidemiol. 127, 353–364 (1988).
Google Scholar
Keitel, W. A., Cate, T. R., Couch, R. B., Huggins, L. L. & Hess, K. R. Efficacy of repeated annual immunization with inactivated influenza virus vaccines over a five year period. Vaccine 15, 1114–1122 (1997).
Google Scholar
Beyer, W. E., de Bruijn, I. A., Palache, A. M., Westendorp, R. G. & Osterhaus, A. D. Protection against influenza after annually repeated vaccination: a meta-analysis of serologic and field studies. Arch. Intern. Med. 159, 182–188 (1999).
Google Scholar
Gostic, K. M., Ambrose, M., Worobey, M. & Lloyd-Smith, J. O. Potent protection against H5N1 and H7N9 influenza via childhood hemagglutinin imprinting. Science 354, 722–726 (2016).
Google Scholar
Gostic, K. M. et al. Childhood immune imprinting to influenza A shapes birth year-specific risk during seasonal H1N1 and H3N2 epidemics. PLoS Pathog. 15, e1008109 (2019).
Google Scholar
Arevalo, P., McLean, H. Q., Belongia, E. A. & Cobey, S. Earliest infections predict the age distribution of seasonal influenza A cases. eLife 9, 19001875 (2020).
Google Scholar
Tsang, T. K. et al. Investigation of the impact of childhood immune imprinting on birth year-specific risk of clinical infection during influenza A virus epidemics in Hong Kong. J. Infect. Dis. 228, 169–172 (2023).
Google Scholar
Koutsakos, M. & Ellebedy, A. H. Immunological imprinting: understanding COVID-19. Immunity 56, 909–913 (2023).
Google Scholar
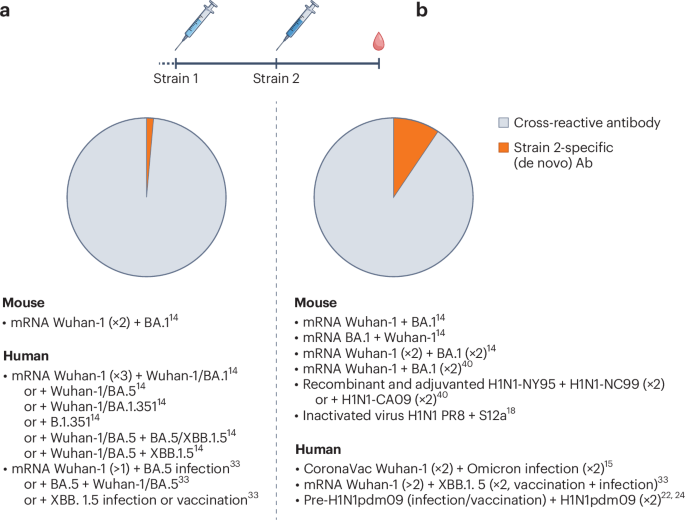
Liang, C.-Y. et al. Imprinting of serum neutralizing antibodies by Wuhan-1 mRNA vaccines. Nature 630, 950–960 (2024).
Google Scholar
Yisimayi, A. et al. Repeated Omicron exposures override ancestral SARS-CoV-2 immune imprinting. Nature 625, 148–156 (2023).
Google Scholar
Kim, J. H., Skountzou, I., Compans, R. & Jacob, J. Original antigenic sin responses to influenza viruses. J. Immunol. 183, 3294–3301 (2009).
Google Scholar
Monto, A. S., Malosh, R. E., Petrie, J. G. & Martin, E. T. The doctrine of original antigenic sin: separating good from evil. J. Infect. Dis. 215, 1782–1788 (2017).
Google Scholar
Linderman, S. L. & Hensley, S. E. Antibodies with ‘original antigenic sin’ properties are valuable components of secondary immune responses to influenza viruses. PLoS Pathog. 12, e1005806 (2016).
Google Scholar
Yewdell, J. W. & Santos, J. J. S. Original antigenic sin: how original? How sinful? Cold Spring Harb. Perspect. Med. 11, a038786 (2021).
Google Scholar
Erbelding, E. J. et al. A universal influenza vaccine: the strategic plan for the National Institute of Allergy and Infectious Diseases. J. Infect. Dis. 218, 347–354 (2018).
Google Scholar
Fonville, J. M. et al. Antibody landscapes after influenza virus infection or vaccination. Science 346, 996–1000 (2014).
Google Scholar
Wrammert, J. et al. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J. Exp. Med. 208, 181–193 (2011).
Google Scholar
Ellebedy, A. H. et al. Induction of broadly cross-reactive antibody responses to the influenza HA stem region following H5N1 vaccination in humans. Proc. Natl Acad. Sci. USA 111, 13133–13138 (2014).
Google Scholar
Andrews, S. F. et al. Immune history profoundly affects broadly protective B cell responses to influenza. Sci. Transl. Med. 7, 316ra192 (2015).
Google Scholar
Hoehn, K. B. et al. Human B cell lineages associated with germinal centers following influenza vaccination are measurably evolving. eLife 10, e70873 (2021).
Google Scholar
Henry, C. et al. Influenza virus vaccination elicits poorly adapted B cell responses in elderly individuals. Cell Host Microbe 25, 357–366 (2019).
Google Scholar
Lee, J. et al. Persistent antibody clonotypes dominate the serum response to influenza over multiple years and repeated vaccinations. Cell Host Microbe 25, 367–376 (2019).
Google Scholar
Lee, J. et al. Molecular-level analysis of the serum antibody repertoire in young adults before and after seasonal influenza vaccination. Nat. Med. 22, 1456–1464 (2016).
Google Scholar
Dugan, H. L. et al. Preexisting immunity shapes distinct antibody landscapes after influenza virus infection and vaccination in humans. Sci. Transl. Med. 12, eabd3601 (2020).
Google Scholar
Teoh, Z. et al. Factors associated with prolonged respiratory virus detection from polymerase chain reaction of nasal specimens collected longitudinally in healthy children in a US birth cohort. J. Pediatr. Infect. Dis. Soc. 13, 189–195 (2024).
Google Scholar
Hoy, G. et al. Increased influenza severity in children in the wake of SARS-CoV-2. Influenza Other Respir. Viruses 17, e13178 (2023).
Google Scholar
Maier, H. E. et al. The Nicaraguan Pediatric Influenza Cohort Study, 2011–2019: influenza incidence, seasonality, and transmission. Clin. Infect. Dis. 76, e1094–e1103 (2023).
Google Scholar
Johnston, T. S. et al. Immunological imprinting shapes the specificity of human antibody responses against SARS-CoV-2 variants. Immunity 57, 912–925 (2024).
Google Scholar
Tortorici, M. A. et al. Persistent immune imprinting occurs after vaccination with the COVID-19 XBB.1.5 mRNA booster in humans. Immunity 57, 904–911 (2024).
Google Scholar
Alsoussi, W. B. et al. SARS-CoV-2 Omicron boosting induces de novo B cell response in humans. Nature 617, 592–598 (2023).
Google Scholar
Addetia, A. et al. Neutralization, effector function and immune imprinting of Omicron variants. Nature 621, 592–601 (2023).
Google Scholar
Carreño, J. M., Singh, G., Simon, V., Krammer, F. & PVI study group. Bivalent COVID-19 booster vaccines and the absence of BA.5-specific antibodies. Lancet Microbe 4, e569 (2023).
Google Scholar
Turner, J. S. et al. Human germinal centres engage memory and naive B cells after influenza vaccination. Nature 586, 127–132 (2020).
Google Scholar
Cobey, S. et al. Poor immunogenicity, not vaccine strain egg adaptation, may explain the low H3N2 influenza vaccine effectiveness in 2012–2013. Clin. Infect. Dis. 67, 327–333 (2018).
Google Scholar
Schiepers, A. et al. Molecular fate-mapping of serum antibody responses to repeat immunization. Nature 615, 482–489 (2023).
Google Scholar
Krammer, F. et al. Antibody responses in seropositive persons after a single dose of SARS-CoV-2 mRNA vaccine. N. Engl. J. Med. 384, 1372–1374 (2021).
Google Scholar
Srivastava, K. et al. SARS-CoV-2-infection- and vaccine-induced antibody responses are long lasting with an initial waning phase followed by a stabilization phase. Immunity 57, 587–599 (2024).
Google Scholar
Rodda, L. B. et al. Imprinted SARS-CoV-2-specific memory lymphocytes define hybrid immunity. Cell 185, 1588–1601 (2022).
Google Scholar
Pape, K. A. et al. High-affinity memory B cells induced by SARS-CoV-2 infection produce more plasmablasts and atypical memory B cells than those primed by mRNA vaccines. Cell Rep. 37, 109823 (2021).
Google Scholar
Auladell, M. et al. Influenza virus infection history shapes antibody responses to influenza vaccination. Nat. Med. 8, 363–372 (2022).
Google Scholar
Khan, K. et al. Omicron infection enhances Delta antibody immunity in vaccinated persons. Nature 607, 356–359 (2022).
Google Scholar
Pušnik, J. et al. Vaccination impairs de novo immune response to Omicron breakthrough infection, a precondition for the original antigenic sin. Nat. Commun. 15, 3102 (2024).
Google Scholar
Thompson, M. G. et al. Effects of repeated annual inactivated influenza vaccination among healthcare personnel on serum hemagglutinin inhibition antibody response to A/Perth/16/2009 (H3N2)-like virus during 2010–11. Vaccine 34, 981–988 (2016).
Google Scholar
Fox, A. et al. Opposing effects of prior infection versus prior vaccination on vaccine immunogenicity against influenza A(H3N2) viruses. Viruses 14, 470 (2022).
Google Scholar
Zost, S. J. et al. Contemporary H3N2 influenza viruses have a glycosylation site that alters binding of antibodies elicited by egg-adapted vaccine strains. Proc. Natl Acad. Sci. USA 114, 12578–12583 (2017).
Google Scholar
Gouma, S. et al. Comparison of human H3N2 antibody responses elicited by egg-based, cell-based, and recombinant protein-based influenza vaccines during the 2017–2018 season. Clin. Infect. Dis. 71, 1447–1453 (2020).
Google Scholar
Flannery, B., Lipsitch, M. & Cobey, S. Reduced effectiveness of repeat influenza vaccination: distinguishing among within-season waning, recent clinical infection, and subclinical infection. J. Infect. Dis. https://doi.org/10.1093/infdis/jiae220 (2024).
Gouma, S. et al. Middle-aged individuals may be in a perpetual state of H3N2 influenza virus susceptibility. Nat. Commun. 11, 4566 (2020).
Google Scholar
Kim, J. H., Davis, W. G., Sambhara, S. & Jacob, J. Strategies to alleviate original antigenic sin responses to influenza viruses. Proc. Natl Acad. Sci. USA 109, 13751–13756 (2012).
Google Scholar
Wang, W. et al. Antigenic cartography using hamster sera identifies SARS-CoV-2 JN.1 evasion seen in human XBB.1.5 booster sera. Preprint at bioRxiv https://doi.org/10.1101/2024.04.05.588359 (2024).
Hobson, D., Curry, R. L., Beare, A. S. & Ward-Gardner, A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. J. Hyg. 70, 767–777 (1972).
Google Scholar
Feng, S. et al. Correlates of protection against symptomatic and asymptomatic SARS-CoV-2 infection. Nat. Med. 27, 2032–2040 (2021).
Google Scholar
Ferdinands, J. M. et al. Waning of vaccine effectiveness against moderate and severe COVID-19 among adults in the US from the VISION network: test negative, case–control study. BMJ 379, e072141 (2022).
Google Scholar
Chemaitelly, H. et al. Waning of BNT162b2 vaccine protection against SARS-CoV-2 infection in Qatar. N. Engl. J. Med. 385, e83 (2021).
Google Scholar
Accorsi, E. K. et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta variants. JAMA 327, 639–651 (2022).
Google Scholar
Tseng, H. F. et al. Effectiveness of mRNA-1273 against SARS-CoV-2 Omicron and Delta variants. Nat. Med. 28, 1063–1071 (2022).
Google Scholar
Garcia-Beltran, W. F. et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell 185, 457–466 (2022).
Google Scholar
Monge, S. et al. Effectiveness of mRNA vaccine boosters against infection with the SARS-CoV-2 Omicron (B.1.1.529) variant in Spain: a nationwide cohort study. Lancet Infect. Dis. 22, 1313–1320 (2022).
Google Scholar
Yang, B. et al. Effectiveness of CoronaVac and BNT162b2 vaccines against severe acute respiratory syndrome coronavirus 2 Omicron BA.2 infections in Hong Kong. J. Infect. Dis. 226, 1382–1384 (2022).
Google Scholar
Zhou, R. et al. Three-dose vaccination-induced immune responses protect against SARS-CoV-2 Omicron BA.2: a population-based study in Hong Kong. Lancet Reg. Health West. Pac. 32, 100660 (2023).
Google Scholar
Lipsitch, M., Goldstein, E., Ray, G. T. & Fireman, B. Depletion-of-susceptibles bias in influenza vaccine waning studies: how to ensure robust results. Epidemiol. Infect. 147, e306 (2019).
Google Scholar
Kahn, R., Schrag, S. J., Verani, J. R. & Lipsitch, M. Identifying and alleviating bias due to differential depletion of susceptible people in postmarketing evaluations of COVID-19 vaccines. Am. J. Epidemiol. 191, 800–811 (2022).
Google Scholar
Ray, G. T. et al. Depletion-of-susceptibles bias in analyses of intra-season waning of influenza vaccine effectiveness. Clin. Infect. Dis. 70, 1484–1486 (2020).
Google Scholar
Skowronski, D. M. et al. A perfect storm: impact of genomic variation and serial vaccination on low influenza vaccine effectiveness during the 2014–2015 season. Clin. Infect. Dis. 63, 21–32 (2016).
Google Scholar
Ohmit, S. E. et al. Influenza vaccine effectiveness in the community and the household. Clin. Infect. Dis. 56, 1363–1369 (2013).
Google Scholar
Jones-Gray, E., Robinson, E. J., Kucharski, A. J., Fox, A. & Sullivan, S. G. Does repeated influenza vaccination attenuate effectiveness? A systematic review and meta-analysis. Lancet Respir. Med. 11, 27–44 (2023).
Google Scholar
Ohmit, S. E. et al. Influenza vaccine effectiveness in the 2011–2012 season: protection against each circulating virus and the effect of prior vaccination on estimates. Clin. Infect. Dis. 58, 319–327 (2013).
Google Scholar
McLean, H. Q. et al. Impact of repeated vaccination on vaccine effectiveness against influenza A(H3N2) and B during 8 seasons. Clin. Infect. Dis. 59, 1375–1385 (2014).
Google Scholar
Valenciano, M. et al. Vaccine effectiveness in preventing laboratory-confirmed influenza in primary care patients in a season of co-circulation of influenza A(H1N1)pdm09, B and drifted A(H3N2), I-MOVE Multicentre Case–Control Study, Europe 2014/15. Euro Surveill. 21, 30139 (2016).
Google Scholar
Chemaitelly, H. et al. Long-term COVID-19 booster effectiveness by infection history and clinical vulnerability and immune imprinting: a retrospective population-based cohort study. Lancet Infect. Dis. 23, 816–827 (2023).
Google Scholar
Shrestha, N. K. et al. Effectiveness of the coronavirus disease 2019 bivalent vaccine. Open Forum Infect. Dis. 10, ofad209 (2023).
Google Scholar
Monge, S., Pastor-Barriuso, R. & Hernán, M. A. The imprinting effect of COVID-19 vaccines: an expected selection bias in observational studies. BMJ 381, e074404 (2023).
Hernán, M. A. & Monge, S. Selection bias due to conditioning on a collider. BMJ 381, 1135 (2023).
Google Scholar
Hood, N. et al. Influenza vaccine effectiveness among children: 2011–2020. Pediatrics 151, e2022059922 (2023).
Google Scholar
Shanks, G. D., Hussell, T. & Brundage, J. F. Epidemiological isolation causing variable mortality in island populations during the 1918–1920 influenza pandemic. Influenza Other Respir. Viruses 6, 417–423 (2012).
Google Scholar
Flannery, B. et al. Influence of birth cohort on effectiveness of 2015–2016 influenza vaccine against medically attended illness due to 2009 pandemic influenza A(H1N1) virus in the United States. J. Infect. Dis. 218, 189–196 (2018).
Google Scholar
Skowronski, D. M. et al. Beyond antigenic match: possible agent–host and immuno-epidemiological influences on influenza vaccine effectiveness during the 2015–2016 season in Canada. J. Infect. Dis. 216, 1487–1500 (2017).
Google Scholar
Linderman, S. L. et al. Potential antigenic explanation for atypical H1N1 infections among middle-aged adults during the 2013–2014 influenza season. Proc. Natl Acad. Sci. USA 111, 15798–15803 (2014).
Google Scholar
Huang, K.-Y. A. et al. Focused antibody response to influenza linked to antigenic drift. J. Clin. Invest. 125, 2631–2645 (2015).
Google Scholar
Kissling, E. et al. Low 2018/19 vaccine effectiveness against influenza A(H3N2) among 15–64-year-olds in Europe: exploration by birth cohort. Euro Surveill. 24, 1900604 (2019).
Google Scholar
Skowronski, D. M. et al. Paradoxical clade- and age-specific vaccine effectiveness during the 2018/19 influenza A(H3N2) epidemic in Canada: potential imprint-regulated effect of vaccine (I-REV). Euro Surveill. 24, 1900585 (2019).
Google Scholar
Tangye, S. G., Avery, D. T., Deenick, E. K. & Hodgkin, P. D. Intrinsic differences in the proliferation of naive and memory human B cells as a mechanism for enhanced secondary immune responses. J. Immunol. 170, 686–694 (2003).
Google Scholar
Hebeis, B. J. et al. Activation of virus-specific memory B cells in the absence of T cell help. J. Exp. Med. 199, 593–602 (2004).
Google Scholar
Abbott, R. K. et al. Precursor frequency and affinity determine B cell competitive fitness in germinal centers, tested with germline-targeting HIV vaccine immunogens. Immunity 48, 133–146 (2018).
Google Scholar
Tas, J. M. J. et al. Antibodies from primary humoral responses modulate recruitment of naive B cells during secondary responses. Immunity 55, 1856–1871 (2022).
Google Scholar
Silva, M. et al. Targeted elimination of immunodominant B cells drives the germinal center reaction toward subdominant epitopes. Cell Rep. 21, 3672–3680 (2017).
Google Scholar
Zhang, Y. et al. Germinal center B cells govern their own fate via antibody feedback. J. Exp. Med. 210, 457–464 (2013).
Google Scholar
Cyster, J. G. & Wilson, P. C. Antibody modulation of B cell responses—incorporating positive and negative feedback. Immunity 57, 1466–1481 (2024).
Google Scholar
Viant, C. et al. Antibody affinity shapes the choice between memory and germinal center B cell fates. Cell 183, 1298–1311 (2020).
Google Scholar
Gitlin, A. D., Shulman, Z. & Nussenzweig, M. C. Clonal selection in the germinal centre by regulated proliferation and hypermutation. Nature 509, 637–640 (2014).
Google Scholar
Victora, G. D. et al. Germinal center dynamics revealed by multiphoton microscopy with a photoactivatable fluorescent reporter. Cell 143, 592–605 (2010).
Google Scholar
Schwickert, T. A. et al. A dynamic T cell-limited checkpoint regulates affinity-dependent B cell entry into the germinal center. J. Exp. Med. 208, 1243–1252 (2011).
Google Scholar
Toellner, K.-M., Sze, D. M.-Y. & Zhang, Y. What are the primary limitations in B-cell affinity maturation, and how much affinity maturation can we drive with vaccination? A role for antibody feedback. Cold Spring Harb. Perspect. Biol. 10, a028795 (2018).
Angeletti, D. et al. Outflanking immunodominance to target subdominant broadly neutralizing epitopes. Proc. Natl Acad. Sci. USA 116, 13474–13479 (2019).
Google Scholar
Schaefer-Babajew, D. et al. Antibody feedback regulates immune memory after SARS-CoV-2 mRNA vaccination. Nature 613, 735–742 (2023).
Goodwin, E., Gibbs, J. S., Yewdell, J. W., Eisenlohr, L. C. & Hensley, S. E. Influenza virus antibodies inhibit antigen-specific de novo B cell responses in mice. Preprint at bioRxiv https://doi.org/10.1101/2024.04.12.589218 (2024).
Lanzavecchia, A. Receptor-mediated antigen uptake and its effect on antigen presentation to class II-restricted T lymphocytes. Annu. Rev. Immunol. 8, 773–793 (1990).
Google Scholar
Biavasco, R. & De Giovanni, M. The relative positioning of B and T cell epitopes drives immunodominance. Vaccines 10, 1227 (2022).
Google Scholar
Li, F., Smith, P. & Ravetch, J. V. Inhibitory Fcγ receptor is required for the maintenance of tolerance through distinct mechanisms. J. Immunol. 192, 3021–3028 (2014).
Google Scholar
Smith, D. J., Forrest, S., Ackley, D. H. & Perelson, A. S. Variable efficacy of repeated annual influenza vaccination. Proc. Natl Acad. Sci. USA 96, 14001–14006 (1999).
Google Scholar
Zarnitsyna, V. I., Lavine, J., Ellebedy, A., Ahmed, R. & Antia, R. Multi-epitope models explain how pre-existing antibodies affect the generation of broadly protective responses to influenza. PLoS Pathog. 12, e1005692 (2016).
Google Scholar
Yisimayi, A. et al. Omicron-specific naive B cell maturation alleviates immune imprinting induced by SARS-CoV-2 inactivated vaccine. Preprint at bioRxiv https://doi.org/10.1101/2024.05.13.594034 (2024).
Schiepers, A., Van’t Wout, M. F. L., Hobbs, A., Mesin, L. & Victora, G. D. Opposing effects of pre-existing antibody and memory T cell help on the dynamics of recall germinal centers. Immunity 57, 1618–1628 (2024).
Google Scholar
Tseng, H. F. et al. mRNA-1273 bivalent (original and Omicron) COVID-19 vaccine effectiveness against COVID-19 outcomes in the United States. Nat. Commun. 14, 5851 (2023).
Google Scholar
Lin, D.-Y. et al. Durability of XBB.1.5 vaccines against Omicron subvariants. N. Engl. J. Med. 390, 2124–2127 (2024).
Amitai, A. et al. Defining and manipulating B cell immunodominance hierarchies to elicit broadly neutralizing antibody responses against influenza virus. Cell Syst. 11, 573–588 (2020).
Google Scholar
Wang, S. Optimal sequential immunization can focus antibody responses against diversity loss and distraction. PLoS Comput. Biol. 13, e1005336 (2017).
Google Scholar
Sprenger, K. G., Louveau, J. E., Murugan, P. M. & Chakraborty, A. K. Optimizing immunization protocols to elicit broadly neutralizing antibodies. Proc. Natl Acad. Sci. USA 117, 20077–20087 (2020).
Google Scholar
Desikan, R. et al. Vaccine models predict rules for updating vaccines against evolving pathogens such as SARS-CoV-2 and influenza in the context of pre-existing immunity. Front. Immunol. 13, 985478 (2022).
Google Scholar