Genomics’ latest ground-breaking research, presented at the Bupa Health Symposium, shows that a person’s genetic background is a major factor in BMI and therefore important for understanding obesity risk.
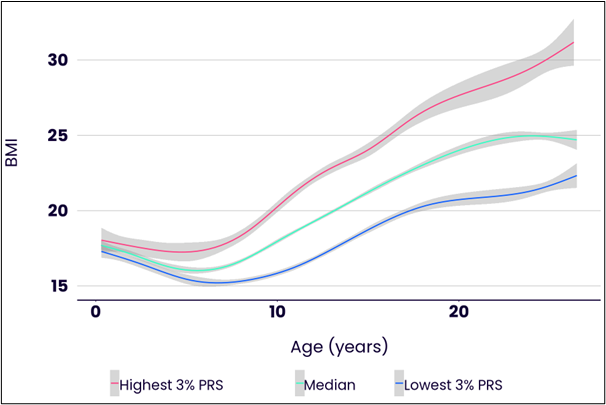
Figure A. Average BMI trajectories from birth to the 20s for individuals in different groups according to genetics. Those with the highest genetic score (top 3% of PRS) are shown in red, those with the median score are shown in green, and those with the lowest genetic score (bottom 3% of PRS) are shown in blue . This figure is based on an analysis of the ALSPAC Longitudinal Study, which followed more than 10,000 children from birth in 1990. Image courtesy: Genomics
Figure B. Average BMI of 10 groups of children at different ages in the ALSPAC study. The group is in the 10th decile of the PRS. The leftmost point in each figure pertains to the 10% of children with the lowest PRS scores, and the second from the left pertains to the 10% of children with the next lowest PRS scores. The rightmost point in each figure pertains to the points with the top 10% of PRS scores. Image credit: Genomics
This new study shows that a person’s BMI, as measured using the polygenic risk score (PRS), is strongly correlated with genetic characteristics from an early age. (See Figures A and B below.) The influence of genetics on BMI becomes more pronounced from early childhood to middle age.
New research shows BMI is strongly influenced by genetics
By the time a child reaches their fourth birthday, BMI is already linked to genetics. Adults in their 20s with relatively high PRS scores for BMI typically experience an increase in BMI over the next 20 years that is three times that of adults with relatively low PRS scores.
Genetics influences everyone’s BMI, starting in early childhood and throughout life. However, it turns out that the influence of genetics in people with unhealthy lifestyles is very large, so the best way to reduce genetics is to work on your lifestyle.
The amount of exercise needed to stabilize your BMI also varies greatly depending on your genetics. For example, people with relatively high genetic risk scores need to walk an average of 10,000 more steps per day to maintain a stable BMI than those with relatively beneficial genetics.
Among people who already suffer from obesity, genetics is a powerful tool for identifying those most at risk for serious complications associated with the condition, such as heart disease and diabetes. Another set of polygenic risk scores can be used to predict the likelihood of obesity. Complications of each of these.
Customized prevention and treatment solutions
Understanding the genetic components of obesity risk is critical to supporting prevention and treatment. Research shows that a healthy lifestyle can prevent obesity and comorbidities, even in people with high genetic risk. Many of the opportunities lie in being able to identify who would benefit most from an intervention, tailor advice to individual needs, and provide each individual with the level of support they need.
A single genetic test provides the opportunity to predict risk for obesity, obesity-related complications, and many other preventable diseases. Genomics has successfully completed a trial in the NHS incorporating the genetic component of cardiovascular disease risk into NHS health checks. Genomics’ PRS for multiple diseases will also be fed back to millions of participants in its flagship Our Future Health program over the next few years. Genomics is currently working with Bupa Health Clinics to introduce tests for four key diseases into health assessments for clinic customers across the UK.
Obesity is the most significant health challenge of the past decade. To discuss it, it is necessary to consider the significant influence of genetics on a person’s predisposition to obesity. We need to change the discourse around overweight from a culture of blame and guilt to how best to help people.
Our research and other researchers have shown that a healthy lifestyle can prevent obesity and comorbidities, even in people at high genetic risk. People at higher risk will need more support to maintain or get back to a healthy weight. We have a tremendous opportunity to develop more sophisticated, personalized, and successful obesity prevention programs.
This is a great example of how incorporating genetics into personalized risk assessments can enable people to become co-pilots, rather than passengers, on their health journeys. We are delighted to be working with Bupa to incorporate this type of information into health assessments for four of the UK’s most preventable diseases. ”
Sir Peter Donnelly Founder and Chief Executive Officer, FRS, FMedSci, Genomics plc