Schnupf, P. & Sansonetti, P. J. Shigella pathogenesis: New insights through advanced methodologies. Bacteria Intracell.1,15–39 (2019).
Troeger, C. et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the global burden of disease study 2016. Lancet. Infect. Dis. 18 (11), 1211–1228 (2018).
Google Scholar
Muthuirulandi Sethuvel, D., Devanga Ragupathi, N., Anandan, S. & Veeraraghavan, B. Update on: Shigella new serogroups/serotypes and their antimicrobial resistance. Lett. Appl. Microbiol.64 (1), 8–18 (2017).
Google Scholar
Halimeh, F. B. et al. Historical, current, and emerging tools for identification and serotyping of Shigella. Braz. J. Microbiol. 5,1–13. (2021).
Nasser, A., Mosadegh, M., Azimi, T. & Shariati, A. Molecular mechanisms of Shigella effector proteins: A common pathogen among diarrheic pediatric population. Mol. Cell. Pediatr.9(1), 12 (2022).
Google Scholar
Mattock, E. & Blocker, A. J. How do the virulence factors of Shigella work together to cause disease?. Front. Cell. Infect. Microbiol.7, 249163 (2017).
Google Scholar
Bajunaid, W. et al. The T3SS of Shigella: Expression, structure, function, and role in vacuole escape. Microorganisms8(12), 1933 (2020).
Google Scholar
Bennish, M. L. & Ahmed, S. Shigellosis. Hunter’s Tropical Medicine and Emerging Infectious Diseases. 492–499 (Elsevier, 2020).
Muthuramalingam, M., Whittier, S. K., Picking, W. L. & Picking, W. D. The Shigella type III secretion system: An overview from top to bottom. Microorganisms. 9 (2), 451 (2021).
Google Scholar
Ali Nor, B. S., Menza, N. C. & Musyoki, A. M. Multidrug-resistant shigellosis among children aged below five years with diarrhea at Banadir hospital in Mogadishu, Somalia. Can. J. Infect. Dis. Med. Microbiol. 2021. (2021).
Assefa, A. & Girma, M. Prevalence and antimicrobial susceptibility patterns of Salmonella and Shigella isolates among children aged below five years with diarrhea attending Robe General Hospital and Goba Referral Hospital, South East Ethiopia. Trop. Dis. Travel Med. Vac. 5(1), 19 (2019).
Sharma, A. & Puhar, A. Plaque assay to determine invasion and intercellular dissemination of Shigella flexneri in TC7 human intestinal epithelial cells. Bio-protocol. 9 (13), e3293–e (2019).
Google Scholar
Kotloff, K. L., Riddle, M. S., Platts-Mills, J. A., Pavlinac, P. & Zaidi, A. K. Shigellosis Lancet391(10122), 801–812 (2018).
Google Scholar
Haksar, D. et al. Fighting shigella by blocking its disease-causing toxin. J. Med. Chem.64(9), 6059–6069 (2021).
Google Scholar
Puzari, M., Sharma, M. & Chetia, P. Emergence of antibiotic resistant Shigella species: A matter of concern. J. Infect. Public Health. 11 (4), 451–454 (2018).
Google Scholar
Salleh, M. Z. et al. Prevalence of multidrug-resistant and extended-spectrum beta-lactamase-producing Shigella species in Asia: A systematic review and meta-analysis. Antibiotics. 11 (11), 1653 (2022).
Google Scholar
Ranjbar, R. & Farahani, A. Shigella: Antibiotic-resistance mechanisms and new horizons for treatment. Infect. Drug Resist. 3137–3167 (2019).
Pitisuttithum, P. et al. Clinical trial of an oral live shigella sonnei vaccine candidate, wrss1, in Thai adults. Clin. Vaccine Immunol.23(7), 564–575 (2016).
Google Scholar
Chakraborty, S. et al. Evaluation of the safety, tolerability, and immunogenicity of an oral, inactivated whole-cell Shigella flexneri 2a vaccine in healthy adult subjects. Clin. Vaccine Immunol.23(4), 315–325 (2016).
Google Scholar
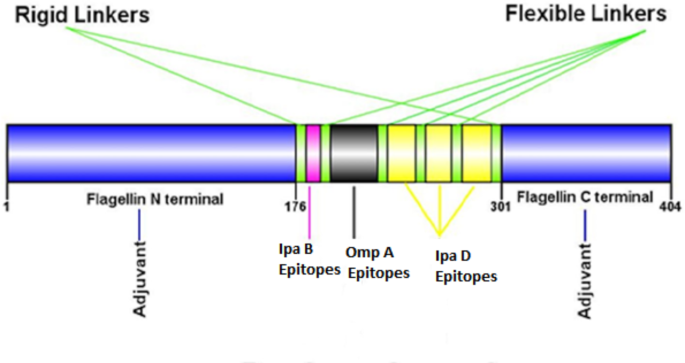
Farhani, I., Nezafat, N. & Mahmoodi, S. Designing a novel multi-epitope peptide vaccine against pathogenic Shigella spp. based immunoinformatics approaches. Int. J. Pept. Res. Ther.25, 541–553 (2019).
Google Scholar
Riddle, M., Chen, W., Kirkwood, C. & MacLennan, C. Update on vaccines for enteric pathogens. Clin. Microbiol. Infect.24(10), 1039–1045 (2018).
Google Scholar
Organization, W. H. Rotavirus vaccines: WHO position paper–July 2021. Wkly. Epidemiol. Rec. 96 (28), 219–301 (2021).
Organization WH. Guidelines for the production and control of inactivated oral cholera vaccines. WHO Tech. Rep. Ser.924, 129–149 (2004).
Pasetti, M. F., Venkatesan, M. M. & Barry, E. M. Oral Shigella vaccines. Mucosal Vaccines 515 – 356. (2020).
Skwarczynski, M. & Toth, I. Non-invasive mucosal vaccine delivery: Advantages, challenges and the future. Expert Opin. Drug Deliv.17(4), 435–437 (2020).
Google Scholar
Wang, S., Liu, H., Zhang, X. & Qian, F. Intranasal and oral vaccination with protein-based antigens: Advantages, challenges and formulation strategies. Protein Cell6(7), 480–503 (2015).
Google Scholar
Davitt, C. J. & Lavelle, E. C. Delivery strategies to enhance oral vaccination against enteric infections. Adv. Drug Deliv. Rev.91, 52–69 (2015).
Google Scholar
Baruah, N., Ahamad, N., Halder, P., Koley, H. & Katti, D. S. Facile synthesis of multi-faceted, biomimetic and cross-protective nanoparticle-based vaccines for drug-resistant Shigella: A flexible platform technology. J. Nanobiotechnol.21(1), 34 (2023).
Google Scholar
Gilavand, F., Marzban, A., Ebrahimipour, G., Soleimani, N. & Goudarzi, M. Designation of chitosan nano-vaccine based on MxiH antigen of Shigella flexneri with increased immunization capacity. Carbohydr. Polym.232, 115813 (2020).
Google Scholar
Camacho, A., Irache, J., De Souza, J., Sánchez-Gómez, S. & Gamazo, C. Nanoparticle-based vaccine for mucosal protection against Shigella flexneri in mice. Vaccine. 31 (32), 3288–3294 (2013).
Google Scholar
Osanloo, M. et al. Comparison effects of Ferula gummosa essential oil and Beta-pinene Alginate nanoparticles on human melanoma and breast cancer cells proliferation and apoptotic index in short term normobaric hyperoxic model. BMC Complement. Med. Ther.23(1), 428 (2023).
Google Scholar
Wawrzyńska, E. & Kubies, D. Alginate matrices for protein delivery–A short review. Physiol. Res.67, S319–S34 (2018).
Google Scholar
Hariyadi, D. et al. The potential for production of freeze-dried oral vaccines using alginate hydrogel microspheres as protein carriers. J. Drug Deliv. Sci. Technol.24(2), 178–184 (2014).
Google Scholar
Yang, D. & Jones, K. S. Effect of alginate on innate immune activation of macrophages. J. Biomed. Mater. Res. Part A 90(2), 411–418 (2009).
Sarei, F., Dounighi, N. M., Zolfagharian, H., Khaki, P. & Bidhendi, S. M. Alginate nanoparticles as a promising adjuvant and vaccine delivery system. Indian J. Pharm. Sci.75 (4), 442 (2013).
Google Scholar
Bakhrushina, E. et al. Comparative study of the mucoadhesive properties of polymers for pharmaceutical use. Open. Access. Macedonian J. Med. Sci.8 (A), 639–645 (2020).
Google Scholar
Craig, D. Q. & Tamburic, S. Dielectric analysis of bioadhesive gel systems. Eur. J. Pharm. Biopharm.44 (1), 61–70 (1997).
Google Scholar
Hariyadi, D. M. & Islam, N. Current status of alginate in drug delivery. Adv. Pharmacol. Pharm. Sci.2020 (1), 8886095 (2020).
Google Scholar
Abasalizadeh, F. et al. Alginate-based hydrogels as drug delivery vehicles in cancer treatment and their applications in wound dressing and 3D bioprinting. J. Biol. Eng.14, 1–22 (2020).
Lai, J. et al. Alginate-based encapsulation fabrication technique for drug delivery: An updated review of particle type, formulation technique, pharmaceutical ingredient, and targeted delivery system. Pharmaceutics. 16 (3), 370 (2024).
Google Scholar
Negahdaripour, M. et al. Structural vaccinology considerations for in silico designing of a multi-epitope vaccine. Infect. Genet. Evol.58, 96–109 (2018).
Google Scholar
Zhang, L. Multi-epitope vaccines: A promising strategy against tumors and viral infections. Cell Mol. Immunol.15 (2), 182–184 (2018).
Google Scholar
Aiman, S. et al. Vaccinomics-aided next-generation novel multi-epitope-based vaccine engineering against multidrug resistant Shigella Sonnei: Immunoinformatics and chemoinformatics approaches. Plos One. 18 (11), e0289773 (2023).
Google Scholar
Nosrati, M. et al. Designing a multi-epitope vaccine for cross-protection against Shigella spp: An immunoinformatics and structural vaccinology study. Mol. Immunol.116, 106–116 (2019).
Google Scholar
Akhgar, S. et al. Immunization of BALB/c mice against Shigella sonnei using a multiepitope protein vaccine through intranasal and subcutaneous administration. Iran. J. Allergy Asthma Immunol. 1–10 (2024).
Chang, A. Y., Chau, V., Landas, J. A. & Pang, Y. Preparation of calcium competent Escherichia coli and heat-shock transformation. JEMI Methods. 1, 22–25 (2017).
Manns, J.M. SDS-polyacrylamide gel electrophoresis (SDS‐PAGE) of proteins. Curr. Protoc. Microbiol.22 (1), A3M1–A3M13 (2011).
Google Scholar
Bradford, M. M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal. Biochem.72 (1–2), 248–254 (1976).
Google Scholar
Valizadeh, A. et al. Alginate nanoparticles containing Lavandula angustifolia essential oil as a potential potent, biocompatible and low-cost antitumor agent. Polym. Bull.81 (2), 1861–1874 (2024).
Google Scholar
Yarian, F. et al. Comparison effects of alginate nanoparticles containing Syzygium aromaticum essential oil and eugenol on apoptotic regulator genes and viability of A-375 and MCF-7 cancer cell lines. BioNanoScience (2023).
Tabynov, K. et al. An intranasal vaccine comprising SARS-CoV-2 spike receptor-binding domain protein entrapped in mannose-conjugated chitosan nanoparticle provides protection in hamsters. Sci. Rep.13 (1), 12115 (2023).
Google Scholar
León, Y. et al. Intranasal immunization of mice with multiepitope chimeric vaccine candidate based on conserved autotransporters SigA, Pic and Sap, confers protection against Shigella flexneri. Vaccines. 8 (4), 563 (2020).
Google Scholar
Chitradevi, S., Kaur, G., Sivaramakrishna, U., Singh, D. & Bansal, A. Development of recombinant vaccine candidate molecule against Shigella infection. Vaccine. 34 (44), 5376–5383 (2016).
Google Scholar
Pavia, D. L., Lampman, G. M., Kriz, G. S. & Vyvyan, J. R. Introduction to Spectroscopy. (2015).
Najwa, M. H. & Solehah, N. N. (eds) Encapsulation of protein within alginate-inulin matrix for targeted drug delivery system. J. Phys. Conf. Ser. (IOP Publishing) (2020).
Osanloo, M., Eskandari, Z., Zarenezhad, E., Qasemi, H. & Nematollahi, A. Studying the microbial, chemical, and sensory characteristics of shrimp coated with alginate sodium nanoparticles containing Zataria multiflora and Cuminum cyminum essential oils. Food Sci. Nutr.11 (6), 2823–2837 (2023).
Google Scholar
Yarian, F. et al. Comparison effects of alginate nanoparticles containing syzygium aromaticum essential oil and eugenol on apoptotic regulator genes and viability of A-375 and MCF-7 cancer cell lines. BioNanoScience. 13 (3), 911–919 (2023).
Google Scholar
Moradi Bidhendi, S. et al. Design and evaluate alginate nanoparticles as a protein delivery system. Arch. Razi Inst.68 (2), 139–146 (2013).
Mitrevej, A., Sinchaipanid, N., Rungvejhavuttivittaya, Y. & Kositchaiyong, V. Multiunit controlled-release diclofenac sodium capsules using complex of chitosan with sodium alginate or pectin. Pharm. Dev. Technol.6 (3), 385–392 (2001).
Google Scholar
Aslam, A. & Okafor, C. N. Shigella StatPearls (Internet) (StatPearls Publishing, 2022).
Holmgren, J. & Lundgren, A. Diarrhea Caused by Bacteria. 252–260.e4 (Elsevier, 2018).
Goumari, M. M., Farhani, I., Nezafat, N. & Mahmoodi, S. Multi-epitope vaccines (MEVs), as a novel strategy against infectious diseases. Curr. Proteom. 17 (5), 354–364 (2020).
Google Scholar
Mahapatra, S. R., Dey, J., Raj, T. K., Misra, N. & Suar, M. Designing a next-generation multiepitope-based vaccine against Staphylococcus aureus using reverse vaccinology approaches. Pathogens. 12 (3), 376 (2023).
Google Scholar
Jafari, E. & Mahmoodi, S. Design, expression, and purification of a multi-epitope vaccine against Helicobacter Pylori based on Melittin as an adjuvant. Microb. Pathog.157, 104970 (2021).
Google Scholar
Oladipo, E. K. et al. Bioinformatics analysis of structural protein to approach a vaccine candidate against Vibrio cholerae infection. Immunogenetics. 75 (2), 99–114 (2023).
Google Scholar
Beikzadeh, B. Immunoinformatics design of multi-epitope vaccine using OmpA, OmpD and enterotoxin against non-typhoidal salmonellosis. BMC Bioinform.24 (1), 63 (2023).
Google Scholar
Feng, F. et al. Strategies to develop a mucosa-targeting vaccine against emerging infectious diseases. Viruses. 14 (3), 520 (2022).
Google Scholar
Desalegn, G. et al. Shigella virulence protein VirG is a broadly protective antigen and vaccine candidate. npj Vaccines. 9 (1), 2 (2024).
Google Scholar
Li, M. et al. Mucosal vaccines: strategies and challenges. Immunol. Lett.217, 116–125 (2020).
Google Scholar
Ramirez, J. E. V., Sharpe, L. A. & Peppas, N. A. Current state and challenges in developing oral vaccines. Adv. Drug Deliv. Rev.114, 116–131 (2017).
Google Scholar
Jazayeri, S. D., Lim, H. X., Shameli, K., Yeap, S. K. & Poh, C. L. Nano and microparticles as potential oral vaccine carriers and adjuvants against infectious diseases. Front. Pharmacol.12, 682286 (2021).
Google Scholar
Pati, R., Shevtsov, M. & Sonawane, A. Nanoparticle vaccines against infectious diseases. Front. Immunol.9, 385476 (2018).
Google Scholar
Karandikar, S., Mirani, A., Waybhase, V., Patravale, V. B. & Patankar, S. Nanovaccines for Oral Delivery-Formulation Strategies and Challenges. 263–293 (Elsevier, 2017).
Shtenberg, Y. et al. Mucoadhesive alginate pastes with embedded liposomes for local oral drug delivery. Int. J. Biol. Macromol.111, 62–69 (2018).
Google Scholar
Downs, E. C., Robertson, N. E., Riss, T. L. & Plunkett, M. L. Calcium alginate beads as a slow-release system for delivering angiogenic molecules in vivo and in vitro. J. Cell. Physiol.152 (2), 422–429 (1992).
Google Scholar
Draget, K. I. & Taylor, C. Chemical, physical and biological properties of alginates and their biomedical implications. Food Hydrocoll.25 (2), 251–256 (2011).
Google Scholar
Zhu, C. et al. Characterization and evaluation of an oral vaccine via nano-carrier for surface immunogenic protein (sip) delivery against Streptococcus agalactiae infection. Int. J. Biol. Macromol.235, 123770 (2023).
Google Scholar
Oliveira, C. R. et al. A new strategy based on SmRho protein loaded chitosan nanoparticles as a candidate oral vaccine against schistosomiasis. PLoS Negl. Trop. Dis.6 (11), e1894 (2012).
Google Scholar
Nevagi, R. J. et al. Polyglutamic acid-trimethyl chitosan-based intranasal peptide nano-vaccine induces potent immune responses against group a streptococcus. Acta Biomater.80, 278–287 (2018).
Google Scholar
Pumchan, A. et al. A novel efficient piscine oral nano-vaccine delivery system: modified halloysite nanotubes (HNTs) preventing streptococcosis disease in tilapia (Oreochromis Sp). Vaccines. 10 (8), 1180 (2022).
Google Scholar
Singh, B. et al. Attuning hydroxypropyl methylcellulose phthalate to oral delivery vehicle for effective and selective delivery of protein vaccine in ileum. Biomaterials. 59, 144–159 (2015).
Google Scholar
Rizvi, S. A. & Saleh, A. M. Applications of nanoparticle systems in drug delivery technology. Saudi Pharm. J.26 (1), 64–70 (2018).
Google Scholar
Banerjee, A., Qi, J., Gogoi, R., Wong, J. & Mitragotri, S. Role of nanoparticle size, shape and surface chemistry in oral drug delivery. J. Controlled Release. 238, 176–185 (2016).
Google Scholar
Roberts, D. L. & Mitchell, J. P. Measurement of aerodynamic particle size distribution of orally inhaled products by cascade impactor: How to let the product specification drive the quality requirements of the cascade impactor. AAPS PharmSciTech. 20 (2), 57 (2019).
Google Scholar
Esmaeili, F. et al. Anti-inflammatory and anti-nociceptive effects of cinnamon and clove essential oils nanogels: An in vivo study. BMC Complement. Med. Ther.22 (1), 143 (2022).
Google Scholar
Manan, F. A. A. et al. Drug release profiles of Mitomycin C encapsulated quantum dots-chitosan nanocarrier system for the possible treatment of non-muscle invasive bladder cancer. Pharmaceutics; 13(9). (2021).
Wei, W. et al. Chitosan nanoparticles loaded with truncated ORF2 protein as an oral vaccine candidate against hepatitis E. Macromol. Biosci.21 (4), 2000375 (2021).
Google Scholar
Ndungo, E. & Pasetti, M. F. Functional antibodies as immunological endpoints to evaluate protective immunity against Shigella. Hum. Vaccines Immunother. 16 (1), 197–205 (2020).
Google Scholar
Toapanta, F. R., Bernal, P. J., Kotloff, K. L., Levine, M. M. & Sztein, M. B. T cell mediated immunity induced by the live-attenuated Shigella flexneri 2a vaccine candidate CVD 1208S in humans. J. Transl. Med.16, 1–17 (2018).
Google Scholar
Le-Barillec, K. et al. Roles for T and NK cells in the innate immune response to Shigella flexneri. J. Immunol.175 (3), 1735–1740 (2005).
Google Scholar
Jehl, S. P. et al. Antigen-specific CD8 + T cells fail to respond to Shigella flexneri. Infect. Immun.79 (5), 2021–2030 (2011).
Google Scholar
Michael, S., Zakaria, N. M., Abbas, M. A., Abdullah, H. & Suppian, R. Immunomodulatory effects of asiaticoside against shigella flexneri-infected macrophages. Trop. life Sci. Res.32 (2), 29 (2021).
Google Scholar
Lodoen, M. B. & Lanier, L. L. Natural killer cells as an initial defense against pathogens. Curr. Opin. Immunol.18 (4), 391–398 (2006).
Google Scholar
Way, S. S., Borczuk, A. C. & Goldberg, M. B. Thymic independence of adaptive immunity to the intracellular pathogen Shigella flexneri serotype 2a. Infect. Immun.67 (8), 3970–3979 (1999).
Google Scholar
Anam, K. et al. Shigella flexneri vaccine development: oral administration of peptides derived from the 49.8 kDa pili protein subunit activates the intestinal immune response in mice. Vet. World. 15 (2), 281 (2022).
Google Scholar
Yagnik, B., Sharma, D., Padh, H. & Desai, P. Oral immunization with LacVax® OmpA induces protective immune response against Shigella flexneri 2a ATCC 12022 in a murine model. Vaccine. 37 (23), 3097–3105 (2019).
Google Scholar
Martinez-Becerra, F. J. et al. Characterization of a novel fusion protein from IpaB and IpaD of Shigella spp. and its potential as a Pan-shigella vaccine. Infect. Immun.81 (12), 4470–4477 (2013).
Google Scholar
Koppolu, B. & Zaharoff, D. A. The effect of antigen encapsulation in chitosan particles on uptake, activation and presentation by antigen presenting cells. Biomaterials. 34 (9), 2359–2369 (2013).
Google Scholar
Kim, C. G., Kye, Y-C. & Yun, C-H. The role of nanovaccine in cross-presentation of antigen-presenting cells for the activation of CD8 + T cell responses. Pharmaceutics. 11 (11), 612 (2019).
Google Scholar
Thakur, A., Mikkelsen, H. & Jungersen, G. Intracellular pathogens: host immunity and microbial persistence strategies. J. Immunol. Res.2019 (1), 1356540 (2019).
Google Scholar
Bhaumik, U. et al. A tetravalent Shigella outer membrane vesicles based candidate vaccine offered cross-protection against all the serogroups of Shigella in adult mice. Microbes Infect.25 (5), 105100 (2023).
Google Scholar
Desalegn, G. et al. A novel Shigella O-polysaccharide–IpaB conjugate vaccine elicits robust antibody responses and confers protection against multiple Shigella serotypes. Msphere. 8 (3), e00019–23 (2023).
Google Scholar