Ryan, M. et al. Distinct T-cell subtypes induced with whole cell and acellular pertussis vaccines in children. Immunology 93, 1 (1998).
Google Scholar
Warfel, J. M., Zimmerman, L. I. & Merkel, T. J. Comparison of three whole-cell pertussis vaccines in the baboon model of pertussis. Clin. Vacc. Immunol. 23, 47–54 (2016).
Google Scholar
Wilk, M. M. et al. Immunization with whole cell but not acellular pertussis vaccines primes CD4 TRM cells that sustain protective immunity against nasal colonization with Bordetella pertussis. Emerg. Microbes Infect. 8, 169–185 (2019).
Google Scholar
Mills, K. H. G., Barnard, A., Watkins, J. & Redhead, K. Cell-mediated immunity to Bordetella pertussis: role of Th1 cells in bacterial clearance in a murine respiratory infection model. Infect. Immun. 61, 399–410 (1993).
Google Scholar
Warfel, J. M. & Merkel, T. J. Bordetella pertussis infection induces a mucosal IL-17 response and long-lived Th17 and Th1 immune memory cells in nonhuman primates. Mucosal Immunol. 6, 787–796 (2013).
Google Scholar
Rowe, J. et al. Antigen-specific responses to diphtheria-tetanus-acellular pertussis vaccine in human infants are initially Th2 polarized. Infect. Immun. 68, 3873–3877 (2000).
Google Scholar
Rowe, J. et al. Th2-associated local reactions to the acellular diphtheria-tetanus-pertussis vaccine in 4- to 6-year-old children. Infect. Immun. 73, 8130–8135 (2005).
Google Scholar
White, O. J. et al. Th2-polarisation of cellular immune memory to neonatal pertussis vaccination. Vaccine 28, 2648–2652 (2010).
Google Scholar
Dubois, V. et al. Suppression of mucosal Th17 memory responses by acellular pertussis vaccines enhances nasal Bordetella pertussis carriage. NPJ Vacc. 6, 6 (2021).
Google Scholar
Kolls, J. K. & Khader, S. A. The role of Th17 cytokines in primary mucosal immunity. Cytokine Growth Factor Rev. 21, 443–448 (2010).
Google Scholar
Borkner, L., Curham, L. M., Wilk, M. M., Moran, B. & Mills, K. H. G. IL-17 mediates protective immunity against nasal infection with Bordetella pertussis by mobilizing neutrophils, especially Siglec-F+ neutrophils. Mucosal Immunol. 14, 1183 (2021).
Google Scholar
Gorringe, A. R. et al. Phase I safety and immunogenicity study of a candidate meningococcal disease vaccine based on Neisseria lactamica outer membrane vesicles. Clin. Vaccin. Immunol. 16, 1113–1120 (2009).
Google Scholar
Nieves, W. et al. A naturally derived outer-membrane vesicle vaccine protects against lethal pulmonary Burkholderia pseudomallei infection. Vaccine 29, 8381–8389 (2011).
Google Scholar
Baker, S. M. et al. A Burkholderia pseudomallei Outer Membrane Vesicle Vaccine Provides Cross Protection against Inhalational Glanders in Mice and Non-Human Primates. Vaccines (Basel) 5, 49 (2017).
Google Scholar
Byvalov, A. A., Konyshev, I. V., Uversky, V. N., Dentovskaya, S. V. & Anisimov, A. P. Yersinia Outer Membrane Vesicles as Potential Vaccine Candidates in Protecting against Plague. Biomolecules 10, 1–23 (2020).
Google Scholar
Wang, X. et al. Remodeling Yersinia pseudotuberculosis to generate a highly immunogenic outer membrane vesicle vaccine against pneumonic plague. Proc. Natl. Acad. Sci. USA 119, 11 (2022).
Bottero, D. et al. Characterization of the immune response induced by pertussis OMVs-based vaccine. Vaccine 34, 3303–3309 (2016).
Google Scholar
Carriquiriborde, F. et al. Pertussis Vaccine Candidate Based on Outer Membrane Vesicles Derived From Biofilm Culture. Front. Immunol. 12, 1 (2021).
Google Scholar
Raeven, R. H. M. et al. The Role of Virulence Proteins in Protection Conferred by Bordetella pertussis Outer Membrane Vesicle Vaccines. Vaccines (Basel) 8, 1–22 (2020).
Elizagaray, M. L. et al. Canonical and Non-canonical Inflammasome Activation by Outer Membrane Vesicles Derived From Bordetella pertussis. Front. Immunol. 11, 1879 (2020).
Google Scholar
Rami, A. et al. Outer Membrane Vesicles of Bordetella pertussis Encapsulated into Sodium Alginate Nanoparticles as Novel Vaccine Delivery System. Curr. Pharm. Des. 27, 4341–4354 (2021).
Google Scholar
Zurita, M. E. et al. A Pertussis Outer Membrane Vesicle-Based Vaccine Induces Lung-Resident Memory CD4 T Cells and Protection against Bordetella pertussis, including Pertactin Deficient Strains. Front Cell Infect. Microbiol. 9, 125 (2019).
Google Scholar
Asensio, C. J. A. et al. Outer membrane vesicles obtained from Bordetella pertussis Tohama expressing the lipid A deacylase PagL as a novel acellular vaccine candidate. Vaccine 29, 1649–1656 (2011).
Google Scholar
Roberts, R. et al. Outer membrane vesicles as acellular vaccine against pertussis. Vaccine 26, 4639–4646 (2008).
Google Scholar
Yılmaz Çolak, Ç. & Tefon Öztürk, B. E. Bordetella pertussis and outer membrane vesicles. Pathog. Glob. Health 117, 342–355 (2023).
Google Scholar
Petersen, H., Nieves, W., Russell-Lodrigue, K., Roy, C. J. & Morici, L. A. Evaluation of a Burkholderia Pseudomallei Outer Membrane Vesicle Vaccine in Nonhuman Primates. Procedia Vaccinol. 8, 38–42 (2014).
Google Scholar
Timothy et al. Bacterial-Derived Outer Membrane Vesicles are Potent Adjuvants that Drive Humoral and Cellular Immune Responses. Pharmaceutics 13, 1–11 (2021).
Baker, S. M. et al. Burkholderia pseudomallei OMVs derived from infection mimicking conditions elicit similar protection to a live-attenuated vaccine. NPJ Vaccines 6, 1–10 (2021).
Google Scholar
Harrell, J. E. et al. An Outer Membrane Vesicle-Adjuvanted Oral Vaccine Protects Against Lethal, Oral Salmonella Infection. Pathogens 10, 626 (2021).
Google Scholar
Gestal, M. C., Howard, L. K., Dewan, K. K. & Harvill, E. T. Bbvac: A Live Vaccine Candidate That Provides Long-Lasting Anamnestic and Th17-Mediated Immunity against the Three Classical Bordetella spp. mSphere 7, 1 (2022).
Google Scholar
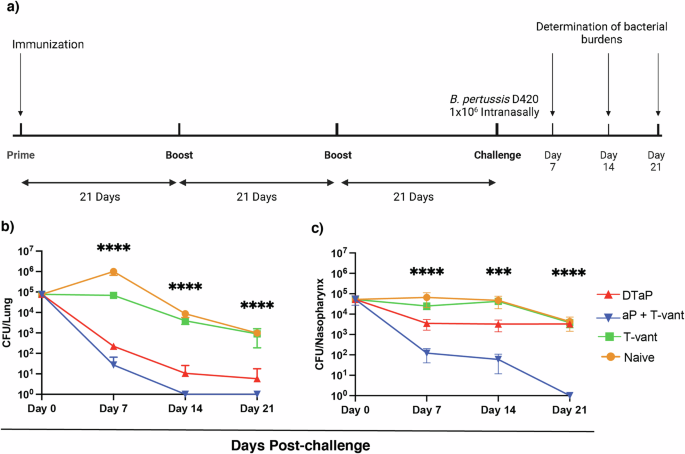
Warfel, J. M., Zimmerman, L. I. & Merkel, T. J. Acellular pertussis vaccines protect against disease but fail to prevent infection and transmission in a nonhuman primate model. Proc. Natl Acad. Sci. 111, 787–792 (2014).
Google Scholar
Steed, L. L., Akporiaye, E. T. & Friedman, R. L. Bordetella pertussis induces respiratory burst activity in human polymorphonuclear leukocytes. Infect. Immun. 60, 2101–2105 (1992).
Google Scholar
Barbic, J., Leef, M. F., Burns, D. L. & Shahin, R. D. Role of gamma interferon in natural clearance of Bordetella pertussis infection. Infect. Immun. 65, 4904–4908 (1997).
Google Scholar
Hellwig, S. M. M., Van Spriel, A. B., Schellekens, J. F. P., Mooi, F. R. & Van de Winkel, J. G. J. Immunoglobulin A-mediated protection against Bordetella pertussis infection. Infect. Immun. 69, 4846–4850 (2001).
Google Scholar
Higgs, R., Higgins, S. C., Ross, P. J. & Mills, K. H. G. Immunity to the respiratory pathogen Bordetella pertussis. Mucosal Immunol. 5, 485–500 (2012).
Google Scholar
Ross, P. J. et al. Relative Contribution of Th1 and Th17 Cells in Adaptive Immunity to Bordetella pertussis: Towards the Rational Design of an Improved Acellular Pertussis Vaccine. PLoS Pathog. 9, e1003264 (2013).
Google Scholar
Redhead, K., Watkins, J., Barnard, A. & Mills, K. H. G. Effective immunization against Bordetella pertussis respiratory infection in mice is dependent on induction of cell-mediated immunity. Infect. Immun. 61, 3190 (1993).
Google Scholar
Chasaide, C. N. & Mills, K. H. G. Next-Generation Pertussis Vaccines Based on the Induction of Protective T Cells in the Respiratory Tract. Vaccines (Basel) 8, 1–28 (2020).
Anderson, K. G. et al. Intravascular staining for discrimination of vascular and tissue leukocytes. Nat. Protoc. 2013 9:1 9, 209–222 (2014).
Zhang, Y. et al. Determination of serum neutralizing antibodies reveals important difference in quality of antibodies against pertussis toxin in children after infection. Vaccine 39, 1826–1830 (2021).
Google Scholar
Acquaye-Seedah, E. et al. Characterization of individual human antibodies that bind pertussis toxin stimulated by acellular immunization. Infect. Immun. 86 (2018).
Nguyen, A. W. et al. Neutralization of pertussis toxin by a single antibody prevents clinical pertussis in neonatal baboons. Sci. Adv. 6 (2020).
Hewlett, E. L. & Halperin, S. A. Serological correlates of immunity to Bordetella pertussis: Editorial. Vaccine 16, 1899–1900 (1998).
Google Scholar
Storsaeter, J., Hallander, H. O., Gustafsson, L. & Olin, P. Levels of anti-pertussis antibodies related to protection after household exposure to Bordetella pertussis. Vaccine 16, 1907–1916 (1998).
Google Scholar
Madhavan, M. et al. Tolerability and immunogenicity of an intranasally-administered adenovirus-vectored COVID-19 vaccine: An open-label partially-randomised ascending dose phase I trial. EBioMed. 85, 104298 (2022).
Google Scholar
WHO. DTaP Immunization Coverage Database. Immunization Data Portal https://immunizationdata.who.int/ (2022).
WHO. Pertussis reported cases and incidence. https://immunizationdata.who.int/pages/incidence/pertussis.html (2022).
Klein, N. P., Bartlett, J., Rowhani-Rahbar, A., Fireman, B. & Baxter, R. Waning Protection after Fifth Dose of Acellular Pertussis Vaccine in Children. N. Engl. J. Med. 367, 1012–1019 (2012).
Google Scholar
De Cellès, M. D., Magpantay, F. M. G., King, A. A. & Rohani, P. The impact of past vaccination coverage and immunity on pertussis resurgence. Sci. Transl. Med. 10 (2018).
Zerbo, O. et al. Acellular Pertussis Vaccine Effectiveness Over Time. Pediatrics 144 (2019).
Damron, F. H. et al. Overcoming Waning Immunity in Pertussis Vaccines: Workshop of the National Institute of Allergy and Infectious Diseases. J. Immunol. 205, 877 (2020).
Google Scholar
Craig, R. et al. Asymptomatic Infection and Transmission of Pertussis in Households: A Systematic Review. Clin. Infect. Dis. 70, 152–161 (2020).
Google Scholar
Allen, A. C. et al. Sustained protective immunity against Bordetella pertussis nasal colonization by intranasal immunization with a vaccine-adjuvant combination that induces IL-17-secreting TRM cells. Mucosal Immunol. 11, 1763–1776 (2018).
Google Scholar
Solans, L. et al. IL-17-dependent SIgA-mediated protection against nasal Bordetella pertussis infection by live attenuated BPZE1 vaccine. https://doi.org/10.1038/s41385-018-0073-9 (2018).
Ryan, M. et al. Bordetella pertussis respiratory infection in children is associated with preferential activation of type 1 T helper cells. J. Infect. Dis. 175, 1246–1250 (1997).
Google Scholar
Mcguirk, P. & Mills, K. H. G. A Regulatory Role for Interleukin 4 in Differential Inflammatory Responses in the Lung following Infection of Mice Primed with Th1- or Th2-Inducing Pertussis Vaccines. Infect. Immun. 68, 1383 (2000).
Google Scholar
Lavelle, E. C. & Ward, R. W. Mucosal vaccines – fortifying the frontiers. Nat. Rev. Immunol. 22, 236–250 (2022).
Google Scholar
Jennings-Gee, J. et al. The Adjuvant Bordetella Colonization Factor A Attenuates Alum-Induced Th2 Responses and Enhances Bordetella pertussis Clearance from Mouse Lungs. Infect. Immun. 86 (2018).
Yount, K. S. et al. Systemic priming and intranasal booster with a BcfA-adjuvanted acellular pertussis vaccine generates CD4+ IL-17+ nasal tissue resident T cells and reduces B. pertussis nasal colonization. Front. Immunol. 14, 1181876 (2023).
Google Scholar
Pschunder, B. et al. Outer membrane vesicles derived from Bordetella pertussis are potent adjuvant that drive Th1-biased response. Front. Immunol. 15, 1387534 (2024).
Google Scholar
Mancini, F. et al. GMMA-Based Vaccines: The Known and The Unknown. Front. Immunol. 12, 715393 (2021).
Google Scholar
Rossi, O., Citiulo, F. & Mancini, F. Outer membrane vesicles: moving within the intricate labyrinth of assays that can predict risks of reactogenicity in humans. Hum. Vaccin Immunother. 17, 1–13 (2021).
Google Scholar
Cheng, K. et al. Bioengineered bacteria-derived outer membrane vesicles as a versatile antigen display platform for tumor vaccination via Plug-and-Display technology. Nat. Commun. 12, 2041 (2021).
Google Scholar
Gaillard, M. E. et al. Acellular pertussis vaccine based on outer membrane vesicles capable of conferring both long-lasting immunity and protection against different strain genotypes. Vaccine 32, 931–937 (2014).
Google Scholar
Raeven, R. H. M. et al. Intranasal immunization with outer membrane vesicle pertussis vaccine confers broad protection through mucosal IgA and Th17 responses. Sci. Rep. 10, 7396 (2020).
Google Scholar
Sidey, F. M., Furman, B. L. & Wardław, A. C. Effect of hyperreactivity to endotoxin on the toxicity of pertussis vaccine and pertussis toxin in mice. Vaccine 7, 237–241 (1989).
Google Scholar
Loscher, C. E., Donnelly, S., McBennett, S., Lynch, M. A. & Mills, K. H. G. Proinflammatory Cytokines in the Adverse Systemic and Neurologic Effects Associated with Parenteral Injection of a Whole Cell Pertussis Vaccine. Ann. N. Y Acad. Sci. 856, 274–277 (1998).
Google Scholar
Armstrong, M. E., Loscher, C. E., Lynch, M. A. & Mills, K. H. G. IL-1β-dependent neurological effects of the whole cell pertussis vaccine: a role for IL-1-associated signalling components in vaccine reactogenicity. J. Neuroimmunol. 136, 25–33 (2003).
Google Scholar
Geurtsen, J. et al. Consequences of the expression of lipopolysaccharide-modifying enzymes for the efficacy and reactogenicity of whole-cell pertussis vaccines. Microbes Infect. 9, 1096–1103 (2007).
Google Scholar
Kumar, P. et al. Intestinal interleukin-17 receptor signaling mediates reciprocal control of the gut microbiota and autoimmune inflammation. Immunity 44, 659 (2016).
Google Scholar
Propst, K. L., Mima, T., Choi, K. H., Dow, S. W. & Schweizer, H. P. A Burkholderia pseudomallei delta purM mutant is avirulent in immunocompetent and immunodeficient animals: candidate strain for exclusion from select-agent lists. Infect. Immun. 78, 3136–3143 (2010).
Google Scholar
Miura, K. et al. ELISA units, IgG subclass ratio and avidity determined functional activity of mouse anti-Pfs230 antibodies judged by a standard membrane-feeding assay with Plasmodium falciparum. Vaccine 37, 2073 (2019).
Google Scholar